Healthier amounts, types and proportions of fats in our blood can be developed with appropriate levels of movement.
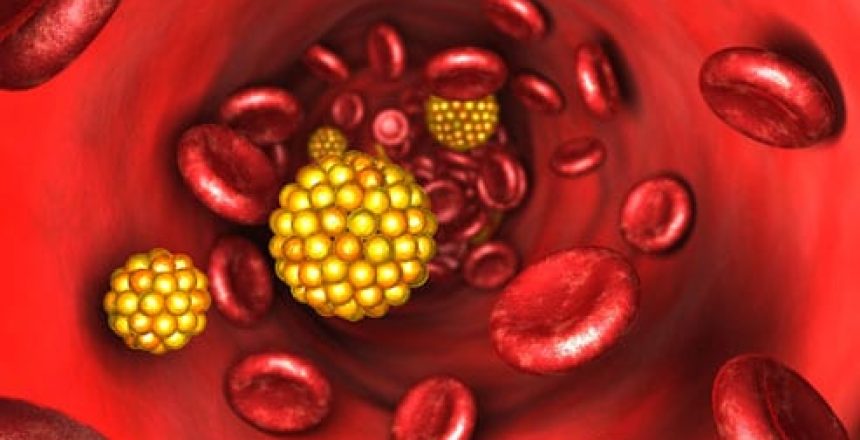
A ‘Lipid’ is the technical name for fats and oils.
Blood lipids are the relative amount and proportion of fats, cholesterol, and other molecules that they form which are found in the blood.
Clearly this is a focus of traditional medicine, particularly in terms of cardiac (heart) health and risk-factors for heart-lung-vessel disease. We often hear about ‘total triglycerides’ ‘LDL and HDL cholesterol’ and more.
Both the liver (which is deeply involved in regulating the fat content in the blood) and the cells which store and release fat to the body (adipocytes) are broadly impacted by exercise (movement) and the types of food we eat, however a body of research now suggests that some changes directly to blood lipids specifically occur in association with exercise itself.
One such change is a genetic expression causing a decrease in an enzyme that helps breakdown fat-carrier molecules. This has specifically been shown to be an effect internal to the cell (ie. direct change in genetic expression) rather than be due to the systemic effect of adrenalin or other hormones. This enzyme decrease leads to a reduced ‘clearance’ of triglyceride-rich lipoproteins.
Also identified has been a change in the expression of genes responsible for transport and burning of fatty acids for energy.
There has been much new research into people becoming ‘fat-adapted’ by using methods such as intermittent fasting and/or a ‘ketogenic’ nutrition plan where fat is burnt as a primary energy source instead of the common state of the body preferentially burning carbohydrate (sugar).
There is a lot of misunderstanding about the actual importance of lipids (because of the faulty science underlying the diet-heart hypothesis).
LDL, vLDL and even the ‘good’ HDL are not themselves ‘cholesterol’ – they are carrier molecules which ‘chaperone’ cholesterol to where it is needed in the body.
Cholesterol is the basis for most of the hormones in our body, as well as Vitamin D. It is also found in the membrane of every cell of our body where it plays critical roles in intercellular communication and signalling.
It is certainly true than certain fractions of LDL cholesterol-carrying molecules can oxidize and accumulate in blood vessel ‘plaques’.
LDL is labelled ‘bad’ because it can release cholesterol like a ‘band-aid’ to try to plug up internal blood vessel injury – however because these cholesterol band-aids then are exposed to the oxygen flowing in the blood around it, it can oxidise and potentially form a plaque. Better movement leads to healthier blood vessels, less likely to be injured or inflamed and therefore less likely to need these cholesterol band-aids.
A deficiency in required movement is perceived by the body as a stressor, which will fire off stress physiology, impacting liver function, and increasing LDL therefore playing a role in the development of cardiovascular disease.
Better movement, in the ways genetically required by our bodies can normalise blood fats and contribute to overall cellular (homeostatic) healthy function.